Brian Hoberman, MD, CIO of The Permanente Federation, on how Kaiser Permanente is maximizing technology to benefit patient care.

Caring for those who provide care
Putting the physician at the center of a wellness culture
First of two parts
By Benjamin Seto
The Permanente Federation
As the health care industry continues to battle with physician burnout, the Permanente Medical Groups have made physician wellness and resilience a key cornerstone to their work to achieve the “Quadruple Aim.”
The Quadruple Aim is based on the more commonly known Triple Aim, which focuses on improving the health of populations, enhancing the care experience for individuals, and reducing per capita cost of health care. The fourth aim puts the spotlight on ensuring the well-being of doctors who provide care.
“Caring for our healers must become part of the culture in health care,” says Edward Ellison, MD, executive medical director and chairman of the Southern California Permanente Medical Group (SCPMG), which serves more than 4.4 million Kaiser Permanente patients in Southern California. “Physicians are often perfectionists who always prioritize others’ needs above their own and this can have serious consequences. We must create an environment that not only offers physicians the right support, but also gives them the space to maintain their own health and well-being.”
Dr. Ellison, who has spoken publicly about the need to address physician burnout, says that although some progress has been made, more needs to be done to ensure it is front and center. “Prioritizing physician wellness, through education, wellness initiatives, and by making our practices and processes more efficient and supportive to physicians, is essential,” he says. “Burnout is an epidemic. We need to drive real change to turn that around.”
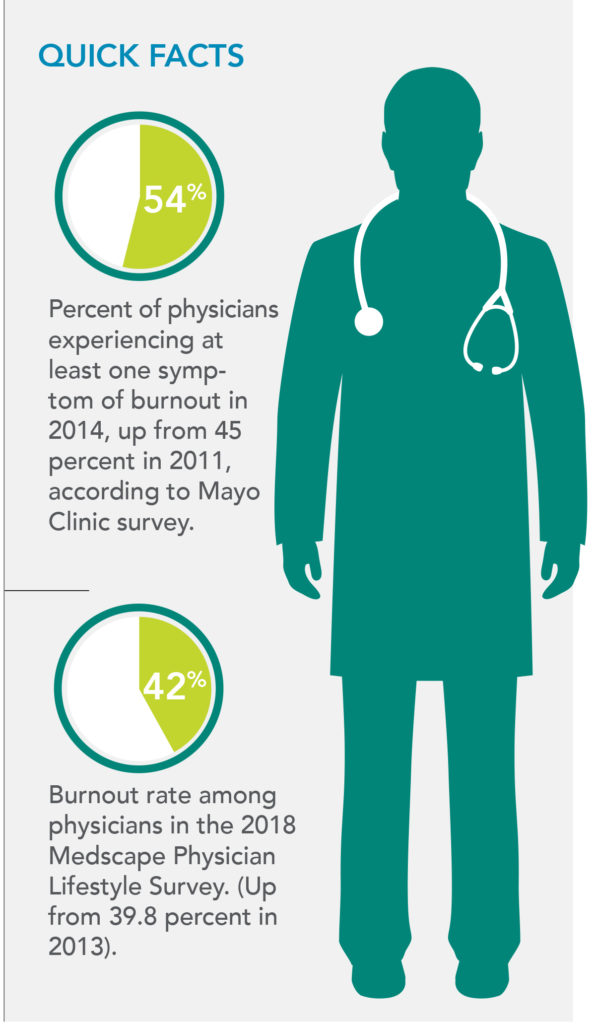 When the AMA and Mayo Clinic conducted a survey in 2011 on burnout and physician satisfaction, about 45 percent of U.S. physicians displayed indicators for burnout. Repeated three years later, the percentage of doctors showing signs of burnout went up (see graphic). A recent study presented at the American Psychiatric Association’s 2018 meeting indicated that U.S. physicians have the highest suicide rate of any profession – even higher than those in the military – with a rate of 28 to 40 suicides per 100,000.
When the AMA and Mayo Clinic conducted a survey in 2011 on burnout and physician satisfaction, about 45 percent of U.S. physicians displayed indicators for burnout. Repeated three years later, the percentage of doctors showing signs of burnout went up (see graphic). A recent study presented at the American Psychiatric Association’s 2018 meeting indicated that U.S. physicians have the highest suicide rate of any profession – even higher than those in the military – with a rate of 28 to 40 suicides per 100,000.
All this raise concerns such as attracting people to pursue a career in medicine and, more importantly, the potential for medical errors. In a study published earlier this summer in Mayo Clinic Proceedings, a survey of more than 6,600 physicians found over 10 percent of doctors reported a “major medical error” in the prior three months that they attributed to burnout.
Sharing best practices on wellness
In light of these staggering numbers, the PMGs are banding together, sharing various approaches to address physician burnout. An Interregional Physician Health and Wellness working group was created encouraging PMGs to adopt programs and policies based on the following:
- Quadruple Aim, based on the Institute for Healthcare Improvement’s Triple Aim.
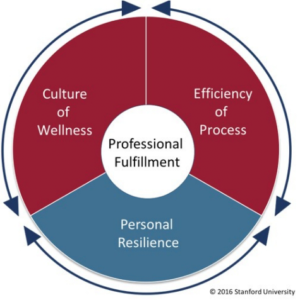
- Stanford Medicine’s WellMD Professional Fulfillment Model that focuses on three domains: culture of wellness, efficiency of practice, and personal resilience.
- The SELF CARE Model – which stands for Sleep, Exercise, Love and Laughter, Food, Compassion, Awe, Resilience, and Engagement – developed by SCPMG and the Hawaii Permanente Medical Group (HPMG).
While most wellness programs often start with personal resilience, the Stanford model gives equal importance to the other two domains – especially the focus on workplace systems and processes that affect a doctor’s work-life integration.
“A lot of what’s suffocating physicians in practices is in the space of practice efficiency,” says David Bell, MD, executive vice president of People and Leadership Strategy at The Permanente Federation and HPMG’s associate medical director of Professional Development and Service. “As a health care organization creates systems to improve care, it needs to look through the lens of how these operational changes affect the people providing the care. If they don’t, people can literally drown in all the processes.”
Lise Barbour, MD, director of Talent Development and Wellness, Colorado Permanente Medical Group (CPMG), says it was an “aha” moment for her group when considering the Stanford model.
“In the past we’ve only been focused on individual resilience offerings, placing the burden on the individual,” she says. “But the Stanford model shows us that’s only one-third of the solution. We have to change our culture and the way we work to really allow for systemic solutions, and shift away from the perception that it’s on the doctor and not really the company’s responsibilities.”
At SCPMG, for example, traditional tasks of primary care physicians such as notifying patients of fecal tests results for colon cancer screenings are now handled by other members of the care team. Several PMGs work closely with IT to improve how clinicians interact with the organization’s massive electronic health record, improving practice efficiency so it doesn’t drain physicians’ time that can be spent on patients.
“Programs aimed at improving personal resilience, such as yoga or meditation, are much better received when we offer them as solutions together with addressing the pain points of our physicians’ experience at work,” says Susan Warwick, MD, medical director, Professional Development and Wellness, Washington Permanente Medical Group (WPMG).
At WPMG, wellness champions located geographically are connecting with physicians on a listening tour to understand how the organization can meet their needs.
To build on an already robust structure of diverse wellness programming and resources for the 9,000 physicians of The Permanente Medical Group (TPMG) in Northern California and 1,200 physicians of the Mid-Atlantic Permanente Medical Group (MAPMG), these two PMGs have incorporated “Joy and Meaning in Medicine” or “JAMM” as a foundational piece of their overall organizational strategy. They’ve incorporated JAMM into their total performance platform along with categories such as “Exceptional Care Experience” and “Operational Excellence.”
“We want our physicians at the center of cohesive teams that use innovative approaches to operations and allow doctors to be doctors.”
– Richard S. Isaacs, MD, FACS
Richard S. Isaacs, MD, FACS, TPMG CEO and executive director and MAPMG president and CEO, says a vital key to fostering wellness, professional satisfaction, and sustainable careers is to adopt a purposeful approach to supporting physicians and staff in their day-to-day work. “We want our physicians at the center of cohesive teams that use innovative approaches to operations and allow doctors to be doctors,” he says.
Ellie Farahabadi, MD, TPMG’s associate executive director of Physician Human Resources and Physician Education, is eager to harness the potential of collaborative leadership to ensure physicians feel engaged, supported, and find opportunities for professional growth. “We understand the importance of leadership and leadership behaviors that promote a culture of physician wellness and joy,” she says. “All of our leaders are being developed with these in mind.”
Amanjot Sethi, MD, TPMG director of Wellness Operations, says he and Dr. Farahabadi are committed to deploying a broad organizational strategy to support JAMM. “We’re striving to weave wellness into our systems and operations,” says Dr. Sethi. “The goal is to shape a culture where physicians can invest more fully in their patients, colleagues, and personal health.”
Implementing SELF CARE
HPMG’s “SELF CARE” model supports the Stanford model’s domain of developing a wellness culture in an organization. The physician group used the “SELF” model first developed by SCPMG (Sleep, Exercise, Love and Laughter, Food) and added the “CARE” component (Compassion, Awe, Resilience, Engagement) to have a positive effect on physicians’ well-being.
Richele Thornburg, executive vice president, People and Leadership Strategy for the Federation and HPMG’s vice president of Strategy, Leadership, and Communications, says HPMG provides its doctors with two paid professional development days that they can take each year. The physician group also sponsors a biennial health and wellness symposium that all physicians are required to attend.
“One of the keys to our approach in promoting and sustaining a culture of wellness and resilience is to give our physicians and providers lots of different options,” Thornburg says. “We all have our own unique wellness needs and wants, so offering a diverse menu of events, programs, and activities within our SELF CARE model allows the individual to explore what works best for her or him.”
Wellness behavior changes
At Northwest Permanente (NWP), its wellness programs are resulting in improvement and behavior change among its nearly 1,500 physicians, clinicians, and administrative staff. One of its main programs is an online “Wellness Passport” where participants get a new passport every quarter with five options of wellness activities to choose from. A small incentive is provided for those who complete at least four activities.
When the medical group surveyed participants earlier this year, 97 percent said they felt their wellness was valued, and 88 percent made a wellness behavior change based on an activity from the Wellness Passport.
“That’s an incredible number of people making a behavior change,” says Ruth Chang, MD, NWP’s chief people officer. “As a primary care physician, I’m trying to convince patients all day to make a healthy behavior change. So it’s encouraging that this online program can drive such positive change among our physicians and administrative staff.”
Dawn Clark, MD, leads the Permanente Interregional Physician Health and Wellness working group and serves as SCPMG’s chief wellness officer, a position created four years ago to tackle the physician burnout issue. She says a culture shift is needed for physicians.
“Asking for help is often seen as a sign of weakness by doctors,” she says. “We’re supposed to be independent and strong. … We need to change that narrative and engage our physicians. We, all together, can be the solution.”


