Nolan Chang, MD and Stephen Parodi, MD, on how innovations will shift both where and how health care is delivered.
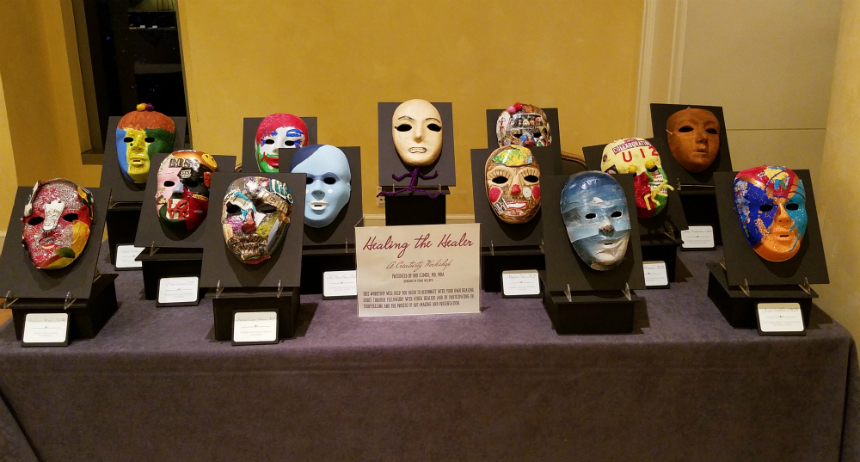
Artwork painted by physicians and clinicians who attended a "Healing the Healers" workshop offered by the The Southeast Permanente Medical Group.
The road to physician wellness
Permanente Medical Groups work to foster culture of wellness and improve physician resilience
Last of two parts
By Benjamin Seto
The Permanente Federation
To address physician burnout, the Permanente Medical Groups, which provide care to Kaiser Permanente members, are collaborating with their doctors to create a culture of wellness and address operational efficiencies to improve the work environment.
On a national level, an Interregional Physician Health and Wellness working group was created encouraging PMGs to adopt programs and policies based on the “Quadruple Aim,” Stanford Medicine’s WellMD Professional Fulfillment Model, and the SELF CARE Model developed by the Southern California Permanente Medical Group (SCPMG) and Hawaii Permanente Medical Group (HPMG).
“Every PMG on its own has been addressing physician burnout for the last few years, with some creating some innovative programs,” says David Bell, MD, executive vice president of People and Leadership Strategy at The Permanente Federation and HPMG’s associate medical director of Professional Development and Service. “But we felt we needed to come together and express a desire in the coming decade to work collectively and support sponsorship of this fundamental work to improve the lives of our physicians.”
Ellie Farahabadi, MD, associate executive director of Physician Human Resources and Physician Education at The Permanente Medical Group (TPMG), adds: “Our goal is to approach wellness through an operational lens. We are collaborating with our operational leaders on optimizing processes, reducing clerical burden, and increasing technology support so that physicians can do the work that brings them joy and meaning.”
The PMGs frame their approach to physician wellness by focusing on one or more of the following:
- The Quadruple Aim: This expands on the Institute for Healthcare Improvement’s Triple Aim, which focuses on improving the health of populations, enhancing the care experience for individuals, and reducing per capita cost of health care. The fourth aim puts the spotlight on ensuring the well-being of doctors who provide care.
- The Stanford model: This focuses on three domains – culture of wellness, efficiency of practice, and personal resilience.
- SELF CARE: The “SELF” model was first developed by SCPMG to emphasize Sleep, Exercise, Love and Laughter, and Food. HPMG added the “CARE” component of Compassion, Awe, Resilience, and Engagement.
- Joy and Meaning in Medicine: This strategic priority utilized by TPMG is designed to support physicians in connecting to their joy and purpose. Leaders across functions and specialties use collaborative leadership to engage physicians and staff in process improvement, community building, and innovative wellness solutions.
“Wellness means different things to different physicians,” says Dawn Clark, MD, SCPMG’s chief wellness officer, a position created four years ago to tackle the physician burnout issue. “We don’t pretend that one thing will fix it. We’re improving resilience through a multi-prong approach.”
Amanjot Sethi, MD, TPMG director of Wellness Operations, agrees. “We have a very diverse medical group – this is seen throughout our people, range of specialties, interests, and generations,” he says. “It’s very important that both our systems and wellness programs are designed to meet a wide spectrum of needs.”
SCPMG, for example, emphasizes SELF CARE with basics such as reminding their doctors about preventive health screenings for themselves. At a doctor’s work anniversary, a reminder letter is sent to close their care gaps. “We’re empowering physicians to care for themselves,” says Dr. Clark, who also leads the Permanente Interregional Physician Health and Wellness working group.
Several PMGs work with their operations teams to address practice efficiencies. For example, some work closely with IT to improve how clinicians interact with the organization’s massive electronic health record, simplifying processes so they don’t drain physicians’ time that can be spent on patients.
“Under the models, both the individual and the organization have responsibilities to make a change,” Dr. Bell says. “What do I own? And what are the ways the medical group and company can work collaboratively to improve and support my career and passions?”
Sharing stories
Several PMGs emphasize the strength of storytelling. Bob Climko, MD, physician program director for Professional Development, The Southeast Permanente Medical Group (TSPMG), says doctors have a long tradition of “narrative medicine,” where storytelling helps to determine a diagnosis.
From the physician’s perspective, sharing stories can help doctors reconnect with the joy of medicine. Dr. Climko has initiated “narrative medicine rounds” at his medical group, where doctors keep a parallel chart to write about a meaningful experience with a patient and then share those stories with colleagues.
“This is a psychological safety zone for our physicians to share their stories,” Dr. Climko says. “It helps them create a bond among colleagues and helps them get in touch with why we became physicians in the first place.”
Wellness means different things to different physicians.
– Dawn Clark, MD, SCPMG chief wellness officer
Colorado has a similar program that’s based on TPMG’s longstanding “Connect to Docs” program, which creates the space and time for clinicians to gather and talk about challenging patient interactions. The discussion isn’t focused on the medical procedures like a typical M&M (morbidity and mortality conferences) but a place to discuss what’s happening in their lives in a non-judgmental environment.
“It’s not a counseling session or therapy session. It’s not a case-review session where there’s criticism,” says Brian Koester, MD, an oncologist who recently retired after 30 years with the Colorado Permanente Medical Group (CPMG). “These sessions were really about understanding your reactions, a patient’s reactions, and different ways to look at a problem.”
Dr. Koester participated in the Connect to Docs sessions at the Oncology Department. He found them so useful while he was practicing that he volunteers today as a facilitator leading these sessions for current oncologists on the team. “Any physician’s job can be difficult, but it’s even more so for oncology where you deal with a lot of sadness,” he says. “This program has allowed us to share some of these emotions. … I wished it was around 20 years ago when I was in the middle of it all.”
Roadmap for physicians
Here’s a sampling of the different programs the PMGs are developing to address the wellness of their doctors:
- Providing practice support. Many TPMG primary care departments are using the Medical Assistant and Physician Partnering (MAPP) program, which provides training for the Physician-MA team including educational programs, engaging in daily huddles, and establishing agreements on standard work. This allows physicians to have greater autonomy in managing their daily practice and delegating the appropriate tasks to their MAs.
- Physicians Helping Physicians. HPMG’s “Physicians Helping Physicians” is a 3-year-old mentor program where doctors are matched with another physician who serves as a coach and mentor. The program has provided needed support for doctors, especially those in primary care, while also opening the eyes of mentors to new growth opportunities.
- Wellness passport. Every 3 months, doctors at Northwest Permanente receive an online “passport” with 5 areas of wellness activities that they can participate in and earn rewards. Participants are encouraged to do at least 4 of the 5 “domains,” which can include activities such as expressing gratitude, practicing mindfulness, or volunteering.
- Reducing work burden. Attempting to reduce physicians’ workloads, SCPMG reorganized duties and used new technology to remove some of the bureaucracy from a doctor’s workday. For example, traditional tasks of primary care physicians like notifying patients of fecal tests results for colon cancer screenings are now handled by other care team members.
- Healing the healers. A quarterly workshop called “Healing the Healers” lets physicians at TSPMG explore their creativity through painting. The goal is to help the doctors connect with themselves along with connecting to fellow workshop participants.
- Leaders embracing wellness. TPMG leadership development programs are being expanded to include a focus on collaborative skills, building trust, effectively leading teams, and highlighting the importance of integrating wellness into operations.
- Rebooting recognition. At CPMG, a wellness committee is reimagining how recognition happens. For example, instead of simply giving a gift or certificate for a doctor’s work anniversary, the committee is planning events that include families to make the recognition more of an experience.
- Wellness Weekends. With a large number of young doctors, the Mid-Atlantic Permanente Medical Group (MAPMG) supports its mentoring program by organizing social events to bring the doctors together to create connections and develop support networks. Activities include participating in an Annual Wellness Weekend event, gathering for happy hours, or attending local sports games.
- Wellness champions. While already in place at several PMGs, physician wellness champions are just formally organizing at the Washington Permanente Medical Group (WPMG), with 12 champions geographically located throughout Washington state where WPMG doctors work. The champions listen to doctors’ concerns and encourage colleagues to share personal stories as a reminder of why they went into medicine.
Five PMGs (Hawaii, Mid-Atlantic, Northwest, Northern California, and Southern California) will also be highlighting their programs during presentations at this fall’s International Conference on Physician Health in Toronto.
“We know there are going to be some doctors who won’t embrace some of these programs in the same manner as others because it may feel touchy-feely,” says Susan Leggett-Johnson, MD, associate medical director for Professional, Leadership and Education Development at MAPMG. “When physicians start to see and feel the impact of building and maintaining connections with colleagues and they understand it’s important from a scientific viewpoint, more may be encouraged to get involved.”
Programs on mindfulness are complemented with helpful training such as SCPMG’s 4-year-old, peer-led program where doctors teach doctors how to efficiently use Kaiser Permanente’s electronic health record. Physicians who’ve taken the training say they’ve shaved off on average 40 minutes of EHR time from their day – another example of one of the many steps in the overall effort to improve a physician’s well-being.
Catch up with the first part of this series here.


