Kaiser Permanente Bernard J. Tyson School of Medicine’s Simulation Center provides hands-on experience in a supportive environment.
Healing the Healers
Working to Reverse Trend of Depression, Burnout Among Medical Students
By Marc H. Klau, Nancy H. Spiegel, and Dawn R. Clark
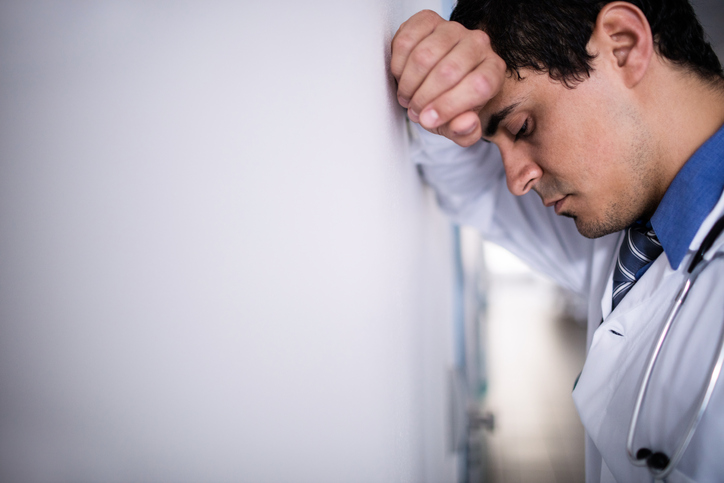
The National Academy of Medicine was frank — and blunt — in an article last year describing the widespread problem of depression, burnout, and suicide among physicians:
“Every year in the United States, about 400 physicians take their own lives — a rate more than double that of the general population. Numerous global studies involving every medical and surgical specialty indicate that approximately 1 in 3 physicians is experiencing burnout at any given time. Medical students appear to be at an equal or higher risk of burnout, depression, substance abuse and suicide.”
Sobering Toll on Medical Students
Medical education’s emotional toll on students has been well documented over the past 15 years. Mayo Clinic studies found nearly half of students surveyed met the criteria for burnout — emotional exhaustion, depersonalization, and low sense of personal accomplishment — and 10 percent had suicidal thinking. We know students come into medical school resilient, gritty, and optimistic and come out less resilient and less optimistic. That decline continues in residency, and these future physicians then enter a practice environment that’s increasingly pressured.
The traditional sink-or-swim culture of medical schools isn’t the right model if our goal is to prepare resilient, competent, and culturally sensitive physicians.
As we prepare to open the Kaiser Permanente School of Medicine in a few years, we’re committed to building a culture of well-being — one that starts with setting a tone of respect and collaboration, and builds wellness and resilience into all elements of the school.
What Needs to Change
The traditional sink-or-swim culture of medical schools isn’t the right model if our goal is to prepare resilient, competent, and culturally sensitive physicians. Characteristics such as perfectionism and a tendency toward self-criticism that are common to many medical students are qualities that make good, thorough, committed physicians. But they are also qualities that make them vulnerable to doubt, guilt and depression.
Heavy academic demands, fatigue due to lack of sleep, and the harsh reality of seriously ill patients, distraught families, and death can be a disabling culture shock.
The training environment can make the difference between student burnout and building resilience. Medical schools across the country, along with accreditation and professional organizations, are implementing programs to improve student well-being and resilience. Many Permanente physicians lived through the old medical school culture and, like us, recognize there’s a better way to educate the next generation of physicians.
Designing a Culture of Well-being
Here are some key features that will help us achieve our vision:
- Faculty and staff development. Focus on student well-being in hiring and onboarding. Clinical psychologist to provide group and individual counseling. Student affairs leader to support wellness and academic success.
- Mentoring and support. Matching students with mentors to guide skills development, professional growth, and work-life balance. Student peer groups to support learning and wellness. Wellness services that include nutrition counseling, access to physical activity, sleep-disorder monitoring, and personal counseling sessions.
- Curriculum. Teaching resilience and coping skills that prepare students to go into the clinical setting, make critical but rapid decisions, and remain adaptable in crisis situations. Safe venues for discussing error or harm, feelings of inadequacy, and dealing with difficult or noncompliant patients. Courses on wellness, nutrition, stress, and chemical and alcohol abuse. Workshops to prepare for exams, interviews, and residency placements. Small, interactive classes to promote engagement.
- Clinical rotations. Longer rotations to foster greater connection to teams and patients. Participation in wellness-focused community service.
- Grading. Pass/no-pass grading based on the ability to apply knowledge.
- Learning technology. Access to a broad range of mobile and computer-assisted technologies to facilitate learning.
- Building design. A healthy building with natural light, individual and small-group spaces, natural environments for reflection and study, and spaces for physical activity. Healthy dining and a demonstration kitchen.
Wellness is the Right Aim
We know that clinician depression and burnout can have serious personal and patient-safety consequences. The School of Medicine’s focus on well-being and resilience builds on our commitment to total health, as well as work by the Permanente Medical Groups to build physician leadership, wellness, and resilience. It’s the right foundation for preparing the next generation of physicians to deliver medical excellence.
Marc H. Klau, MD, MBA, is vice dean of Education and Clinical Integration for the Kaiser Permanente School of Medicine and regional chief of Head and Neck Surgery for the Southern California Permanente Medical Group.
Nancy H. Spiegel, MS, is assistant dean of Education, Clinical Integration, and Wellness for the Kaiser Permanente School of Medicine and executive leader, Medical Education, Wellness, and Leadership Development for the Southern California Permanente Medical Group.
Dawn R. Clark, MD, is an obstetrician-gynecologist and serves as chief facilitator for physician wellness for the Southern California Permanente Medical Group.