Nolan Chang, MD, shares ways Kaiser Permanente is using AI to better the patient experience and reduce physician burnout.

Innovative pregnancy care model surrounds mothers with safety net of support
‘Cocoon’ care program weaves physical, mental, and social health support and services to better meet needs of expectant mothers
By Ruben Rodriguez
The Permanente Federation
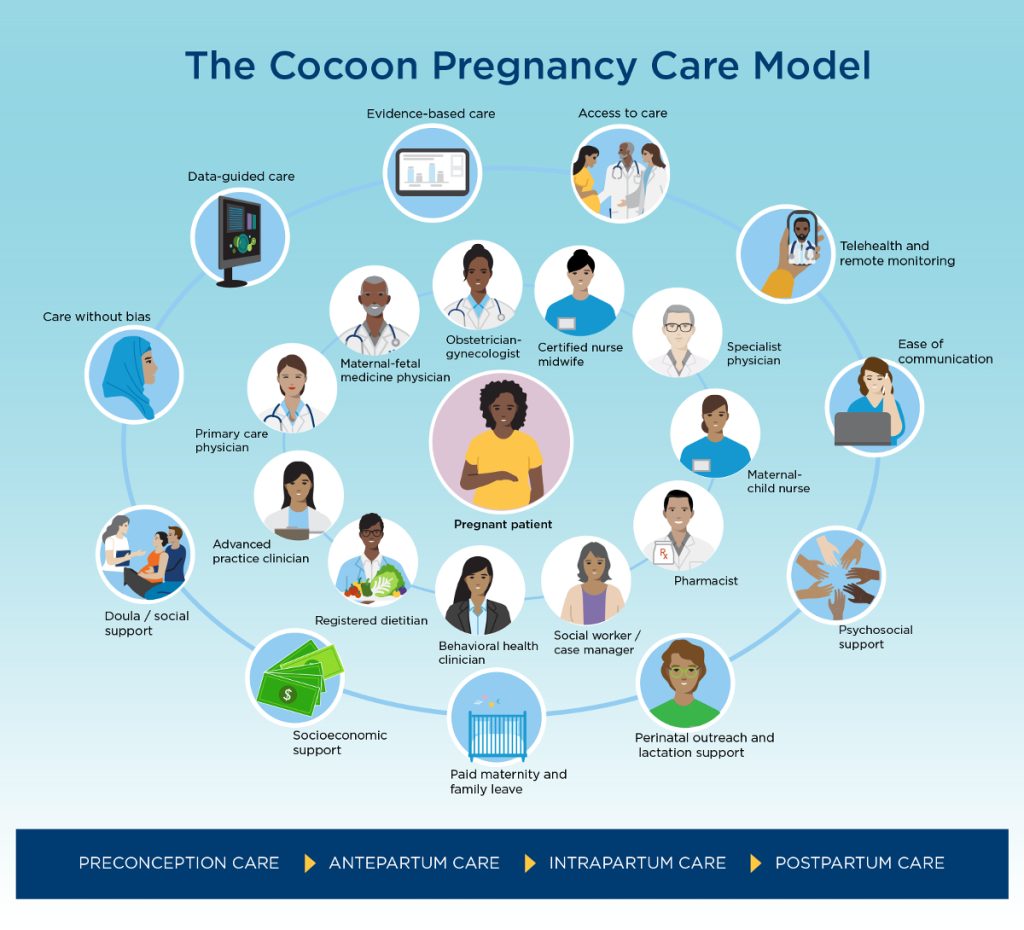
A multidisciplinary team of Permanente physician leaders, certified nurse midwives, and nurse leaders created the Cocoon Pregnancy Care Program to improve the quality of care mothers receive before, during, and after pregnancy, while also addressing the socioeconomic and access issues that burden many women.
Developed within the Women’s Services and Quality and Safety Department at Kaiser Permanente in Georgia, the innovative perinatal care program was recently featured as a case study in the February edition of the New England Journal of Medicine Catalyst.
“This program represents our effort to be a national, state, and local leader in working to reduce health disparities and unnecessary perinatal complications,” says Kate Koplan, MD, MPH, one of the study’s authors. “Leveraging the integrated nature of Kaiser Permanente allowed us to bring together talented teams that already work together into an even more effective unit to improve the quality of care and safety expectant mothers deserve.”
Dr. Koplan serves as chief quality officer and associate medical director for The Southeast Permanente Medical Group, which provides health care for Kaiser Permanente members in Georgia.
Innovating to address a worsening crisis
Global data shows that the U.S. maternal mortality rate continues to exceed that of other high-income countries. And despite increased attention, the Black maternal mortality rate in this country remains a significant public health problem. According to the Centers for Disease Control and Prevention, Black women are 3 times more likely to die from pregnancy-related causes than white women. Many factors contribute to this disparity, including socioeconomic conditions, variations in care, underlying chronic health issues, and structural racism.
The Cocoon Care program exemplifies the power of Permanente Medicine’s integration in improving both the quality of health care and maternal health outcomes.
— Nancy Gin, MD, chief quality officer, The Permanente Federation
To address the multifaceted problems of maternal and infant mortality as well as related health disparities, in January 2019 the team in Georgia embarked on a journey to redesign their perinatal care program. Partnering with analytic teams, they examined past and current data to better understand maternal health demographics, morbidity, and mortality. The perinatal team then contacted other Kaiser Permanente regions and Permanente Medical Groups to learn what they were doing to improve maternal care outcomes and if any best practices could be adapted for the Georgia region. Literature on other evidence-based practices was also reviewed and considered.
By July, the team had enough information to create the Cocoon Pregnancy Care Model. A truly collaborative effort, the program grew to include the participation of adult and family medicine, cardiology, endocrinology, emergency medicine, and behavioral health departments. Operational and leadership teams from nursing practice, IT, pharmacy, and more were also involved.
Improving the care experience with complete specialty care support
What makes the Cocoon Pregnancy Care approach unique is the way traditional and novel elements of maternal care are layered and integrated to meet each expectant mother’s specific needs. The pregnant woman is always at the center of care, protected from harm with appropriate care and services at every stage of pregnancy — preconception, antepartum, intrapartum, and postpartum. These services are provided by a coordinated team of primary, maternal, and specialty care physicians, dietitians, behavioral health clinicians, nurses, social workers, and more.
Although all elements of the multidimensional program are available to pregnant women, some are standard while others are recommended based on a patient’s clinical status and psychosocial needs. Care is tailored to each individual health journey.
“The Cocoon Care program exemplifies the power of Permanente Medicine’s integration in improving both the quality of health care and maternal health outcomes,” says Nancy Gin, MD, executive vice president and chief quality officer of The Permanente Federation. “By bringing together a broad range of health care professionals, from obstetricians to social workers, and employing the best of technology, we can ensure that expectant mothers are getting the holistic, comprehensive, and coordinated care they need throughout their pregnancy journey.”
Adding newer modalities like telehealth, remote monitoring, and psychosocial support to routine maternal care led to improvements in key quality and safety metrics. As described in the NEJM Catalyst case study article, the team moved up the initial postpartum visit from the traditional 4 to 6 weeks after birth to 7 to 10 days after hospital discharge. This change improved screening rates for postpartum complications in all patients from 46 to 85%, and in high-risk patients from 57.5 to 94.3%.
“We paid specific attention to improving postpartum surveillance and screenings, as 40% of maternal deaths occur postpartum,” says Ericka Gibson, MD, MPH, physician program director, Perinatal Safety and Quality for The Southeast Permanente Medical Group and one of the study authors. “By fully integrating disciplines like maternal-child health nurses, behavioral health clinicians, social workers, and case managers — think of them as the fibers of the cocoon — we created a comprehensive perinatal care model that addresses the physical, mental, and social health needs of patients as a means of reducing maternal morbidity and mortality.”
Related story: “Kaiser Permanente plans to offer remote blood pressure monitoring for all pregnancies”
Focus on Black maternal health
 Diabetes and hypertension are known risk factors for maternal mortality and complications such as preeclampsia and preterm birth. A lack of access to screenings and treatment amplifies the problem, especially for Black women who are disproportionately affected by these conditions.
Diabetes and hypertension are known risk factors for maternal mortality and complications such as preeclampsia and preterm birth. A lack of access to screenings and treatment amplifies the problem, especially for Black women who are disproportionately affected by these conditions.
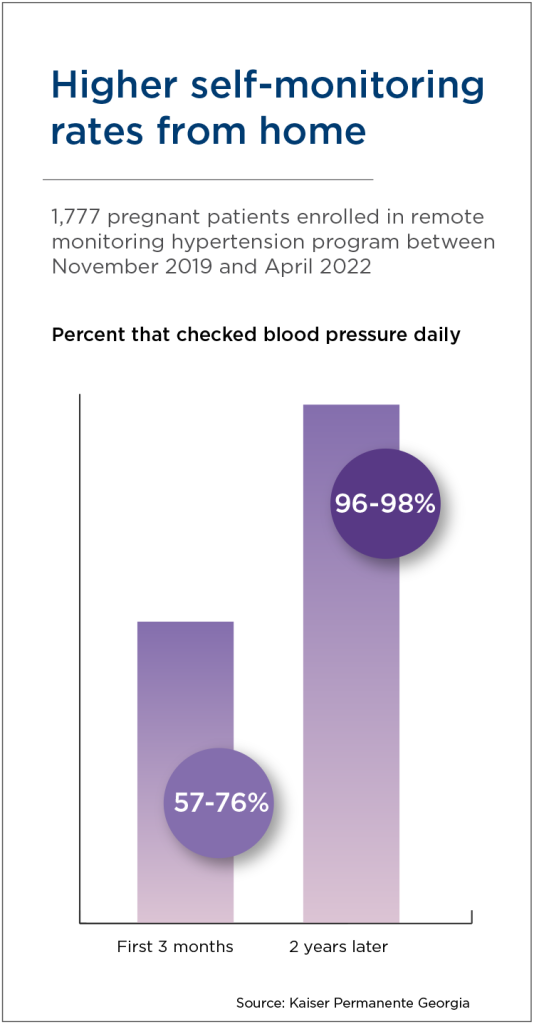
Informed with data from a special obstetric database created in partnership with analysts and statisticians, Permanente physicians identified patients with a high-risk diagnosis for chronic or pregnancy-associated hypertension, as well as for preexisting or gestational diabetes. Mothers were given the option to enroll in a remote monitoring program that made it easier to track their blood pressure and blood sugar levels from the comfort of home. Using Bluetooth-enabled diagnostic tools, the results were transmitted directly to their electronic health record in real time.
Over the course of 18 to 24 months, both programs saw substantial increases in the percentage of enrolled patients who monitored their blood pressure and blood sugar daily. The convenience of remote monitoring and virtual support helps increase the frequency with which mothers track their health measures. This consistency and real-time access to data makes it easier for clinicians to evaluate and respond to abnormal readings, increasing opportunities for interventions.
Providing culturally responsive care is essential to improving Black maternal health. This includes understanding and addressing the social determinants of health that may contribute to health disparities, such as low income and access to healthy food. The Cocoon Care team includes social workers and case managers to support patients with mental health needs, such as stress reduction and other socioeconomic challenges that contribute to health inequities.
“Integration within the health care team and access to our electronic health record system allow for proactive outreach to at-need patients,” says Dr. Gibson. “For instance, we’re able to use neighborhood deprivation scores as markers for individual social health needs and connect patients to social workers or case managers for support.”
In addition, Kaiser Permanente’s Department of Women’s Services hosted a mandatory birth equity training for clinicians and nurses. The training was followed by a series of listening and sharing sessions, creating a safe space for the care team to discuss stories and experience with inequities. The sessions were difficult for some, but they ultimately put the focus on health bias mitigation in health care.
Putting the mother first
As the continues to evolve and improve, the lessons learned are being shared nationally across Kaiser Permanente. Some elements of the program, like remote patient monitoring, are already available to mothers in nearly every Kaiser Permanente region.
According to Dr. Koplan, it’s important to remember that the patient is what matters most. “Connecting the dots to create a holistic experience, bringing pride and leadership opportunities to our care teams, leading with data and safety — all of these things are important to the success of our program,” she says. “Above all, the patient’s voice must be heard, she must feel empowered, supported, and protected.”
Related story: “Driving health care innovation in 10 steps”


