Discover what truly adds value in digital health and AI. Experts discuss ambient AI, chronic disease tools, ROI, policy, and how leaders choose safe, effective innovations.
AI in health care — Physician leaders discuss quest for a strategy
Webinar spotlights AI innovation and its potential to transform care delivery
The potential for artificial intelligence (AI) to innovate health care on a large scale has evaded much of the health care industry, but a panel recently presented by The Permanente Federation said they’re still optimistic about AI’s promise to achieve quality improvements and outcomes for the benefits of patients.
“Right now we’re at a pivotal point where there are an enormous amount of opportunities and directions we can take,” said Vivian S. Lee, MD, PhD, MBA, president of Health Platforms at Verily. “It’s important for us to set the expectations and standards of what we hope to get out of these [AI] tools moving forward.”
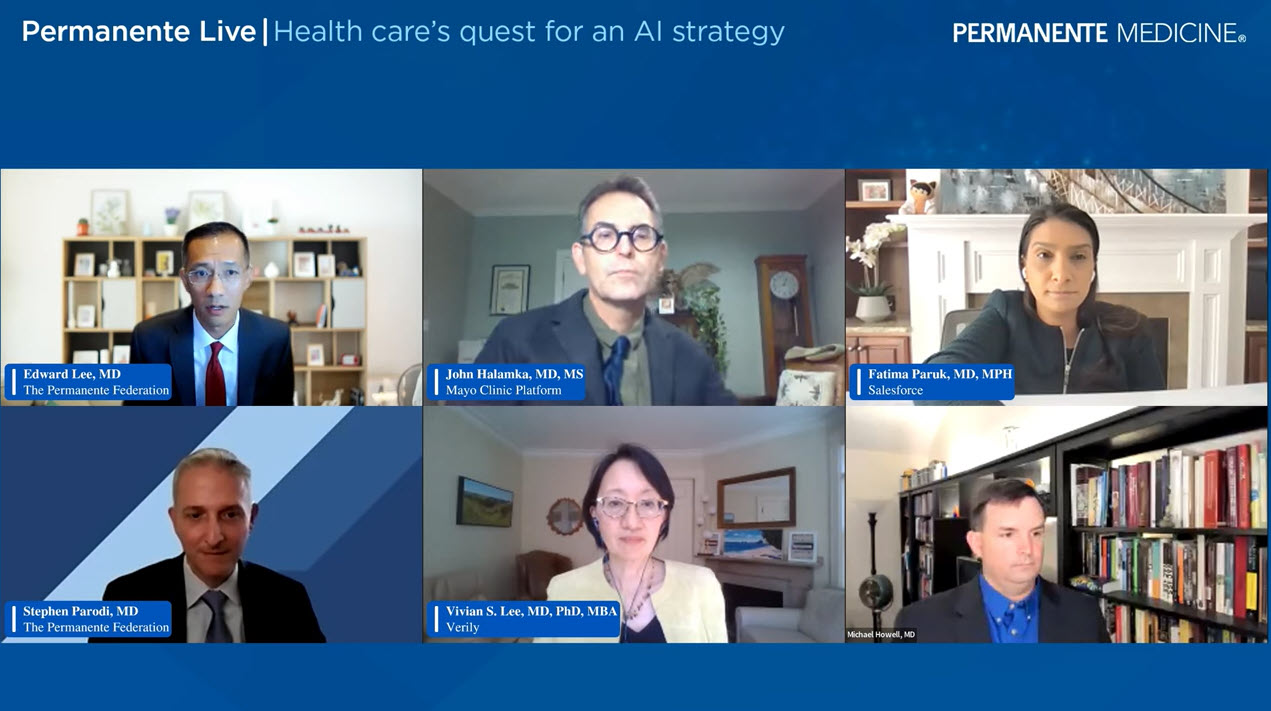
Dr. Lee spoke on the September 26 virtual webinar, “Permanente Live: Health care’s quest for an AI strategy,” along with other physician leaders from health care and technology organizations, including Kaiser Permanente, Mayo Clinic, Google, Verily, and Salesforce. Stephen Parodi, MD, executive vice president of External Affairs, Communications, and Brand at The Permanente Federation, served as moderator.
AI has been the darling of every industry looking to capitalize on the technology to improve services to customers and create cost-efficiencies for companies. AI’s potential in health care resulted in a record $10 billion being invested in digital health startups in 2021 (although the pace has slowed in 2022), according to a Rock Health analysis.
Session panelists said that skepticism is expected and attention needed to be focused on data that serves as the basis for algorithms used to predict care protocols.
Physicians need to “bring [their] native skepticism to the table,” said Michael Howell, MD, chief clinical officer and deputy chief health officer at Google. In collecting and using data, he said it is critical to monitor the process from beginning to end – starting with the conception of an algorithm idea to implementation — to look for potential bias that may contribute to health disparities.
“Care that isn’t equitable isn’t high quality,” Dr. Howell said.
Related story: “Driving health care innovation in 10 steps”
John Halamka, MD, president of Mayo Clinic Platform, said it took Mayo about 2 years to clean and organize the data they used to develop algorithms with their partners. The process included removing identifiers to protect privacy and conducting national and international testing to make sure algorithm models were fair.
“The promise we make to our patients is we use a multilayer defense,” he said, noting, for example, that they don’t allow linking of the data to other databases that could then “re-identify” the data source.
Dr. Halamka also said clinical expertise will be vital to the success of AI. Physicians and clinical leaders need to work with developers to find the right solutions that’ll support patient care. “Working with technologist at their elbow, [physicians] can create models that have clinical relevance, fairness, and utility.”
Edward Lee, MD, executive vice president and chief information officer at the Federation, echoed those comments, saying he often describes AI as “augmented intelligence” that supplements the work of physicians and care teams.
“I think of this technology as a set of tools that assist and augment the physician’s ability to care for patients,” he said. “With AI-augmented care for our physicians and teams, combined with clinical judgment, we create the potential for significant improvement in outcomes for our patients as well as efficiencies for our organization as a whole.”
He shared some examples of how Kaiser Permanente uses AI, including an Advance Alert Monitor program that analyzes hospital patients’ electronic health data to predict when a patient may have a serious decline in health and potentially may need intervention and possibly move to the intensive care unit. Another example of AI use is having computers analyze emails from patients and categorizing the topic. Emails are then sent to the right care team member, providing every member of the care team the freedom to practice at the top of their scope instead of spending time reviewing emails.
I think of this technology as a set of tools that assist and augment the physician’s ability to care for patients.
— Edward Lee, MD, chief information officer, The Permanente Federation
Much of the drive for AI should also come from the patients, said Fatima Paruk, MD, chief health officer and senior vice president at Salesforce. “We realize the patient is going to actually be the empowered patient of the future and demand the change,” she said, adding that Salesforce is working with their partners to create platforms and systems that enable seamless patient access to care.
Dr. Halamka agreed that there’s a change among consumers pushing for advanced technology to improve their health. “The perfect storm for innovation requires technology that’s good enough, policy that’s enabling, and a cultural change that create a sense of urgency,” he said. “There’s a cultural demand of our patients to do this.”
Watch the full replay of the webinar above.