The Smart Messaging Tool helps clinicians better manage patient messages and address high-acuity cases 77% faster.
Reaching Beyond Facilities to Improve Colorectal Cancer Screening

By Theodore Levin, MD, Joanne Schottinger, MD, and Murray Ross
Payers are increasingly using value-based payment to push delivery systems to redefine their product and place. Much has been written about what the new “product” should be, from a hospital stay plus 30 days post-admission, to all the care required by an enrolled or attributed population for a year.
Less has been written about the changing place of health care delivery. Delivery systems are designed to care for people who walk through their doors. However, many value-based payment arrangements hold delivery systems accountable for achieving population health goals, such as cancer screening. These goals can best be met by engaging people who may never enter a medical office.
For most delivery systems, engaging people before they become patients involves a new skill set. In this post, we describe how one large delivery system—Kaiser Permanente—learned to reach beyond its walls to engage healthy members in colorectal cancer (CRC) screening. The organization shifted from an opportunistic screening program that depended on patients entering its physical premises to a proactive program that leveraged opportunities to communicate with and screen members in their homes. These efforts have dramatically improved CRC screening rates, resulting in reduced incidence of colorectal cancer. This experience is relevant for other delivery systems under value-based payment arrangements, which provide financial flexibility to focus on care that happens outside of the traditional “place” of service delivery.
Why is Colorectal Cancer Screening So Important and Effective?
In the United States, colorectal cancer (CRC) is the third-most common cancer and second-leading cause of cancer-related death. More than 49,000 people died of the disease in 2016. Although CRC is highly treatable if caught early, only about two-thirds of Americans aged 50-75 receive the recommended screening. Screening rates among certain populations, particularly Latinos and low-income individuals, are even lower. The National Colorectal Cancer Roundtable set a goal of increasing CRC screening rates in the United States to 80 percent by 2018. Such an improvement would prevent 277,000 new cancers and 203,000 CRC deaths by 2030.
There is clear evidence that three types of CRC screening—colonoscopy, flexible sigmoidoscopy, and fecal occult blood testing (FOBT)—reduce cancer incidence and mortality. These screenings are highly effective because the cancer is slow-growing, and the tests are designed to find both early cancer and pre-cancerous growths called polyps. Polyps can be removed before they turn into cancers.
The most commonly used CRC screening test in the U.S. is colonoscopy, with FOBT a distant second, and flexible sigmoidoscopy third. Colonoscopy and flexible sigmoidoscopy can be burdensome for patients because they are invasive, unpleasant, and require an in-office procedure that interrupts normal activities. These tests also require specialized equipment, dedicated space in a health care facility, and significant health care manpower. In contrast, FOBT is a noninvasive test that patients can perform in their own homes and can be easily processed by health care systems. Though doctors—particularly gastroenterologists—may be more likely to offer colonoscopy than other types of tests, research suggests higher uptake of testing when patients are offered either FOBT or a choice among methods.
In 2002, Medicare began covering colonoscopy for CRC screening, and in 2010, the Affordable Care Act required private health plans to cover CRC screening tests with no patient cost-sharing. With financial barriers removed, it is up to health systems and insurers to encourage patients to get tested. However, most health systems are not set up to do this, as they rely on opportunistic screening, offering tests to patients who are already in the office for a routine visit or when sick.
Meeting Patients Where They Are
Kaiser Permanente, headquartered in Oakland, Calif., is the nation’s largest not-for-profit, integrated delivery system, with more than 11 million patients, 21,000 physicians, and 630 medical offices in eight states and the District of Columbia. A distinctive feature of Kaiser Permanente is that physician groups, the Permanente Medical Groups, receive capitated payments for nearly all services provided to members – an arrangement that many consider a prime example of value-based payment. This post focuses on the activities of Kaiser Permanente in California, which are illustrative of similar activities in all of our regions.
Our efforts to improve CRC screening date back several decades but became more organized beginning in the mid-2000s – around the time the National Committee for Quality Assurance promulgated a CRC screening measure under the Healthcare Effectiveness Data and Information Set (HEDIS). The new HEDIS measure gave us a more accurate read on our CRC screening rates, compared to our previous tracking efforts using patient surveys. We found that we had room for improvement. We knew that most of our primary care physicians were offering sigmoidoscopy (or, in some cases, colonoscopy) to eligible patients, due to an intensive internal education campaign, but patients clearly were not taking them up on the offer in optimal numbers.
In addition, we were aware that CRC screening rates were highest among people with (unrelated) chronic disease, suggesting that our invitation method—in-person, provider recommendation—worked well for people who had frequent contact with our doctors, but not so well for people with less-frequent office visits. We knew we had to develop a screening and communications approach to meet patients where they were—at home—and to provide a screening option that was more convenient.
We accomplished both of these goals through an organized, intensive outreach program around a new type of FOBT – the fecal immunochemical test, also known as a “FIT kit.” This approach separates the screening process from office visits, making it easier to reach patients who are not already in regular contact with a doctor.
Multi-Pronged Outreach
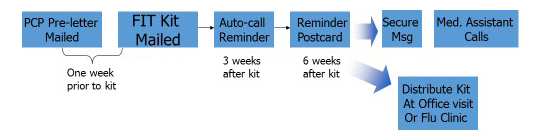
Under the new screening program, patients may still elect to receive colonoscopy or sigmoidoscopy, but most choose the FIT. The FIT kit is a simple test that patients can administer at home. Unlike earlier types of FOBT, it requires only a single sample, which the patient sends directly to a central laboratory for processing in a pre-paid envelope. In all of our regions, the heart of the outreach campaign is a mass mailing of FIT kits to the target population (average-risk adults ages 50 to 75 who are due for screening), identified using population health management tools in the electronic health record (EHR). Initially, we simply mailed kits to patients, followed by a reminder letter several weeks later. Response rates were not as high as we would have liked, so we created a multi-pronged communications strategy around the FIT kit mailing (Figure 1). The strategy includes tactics such as:
- A letter from the patient’s primary care provider, sent one week prior to the FIT kit mailing;
- An auto-call reminder three weeks after the mailing;
- A reminder postcard sent six weeks after the mailing; and,
- If needed, secure email messaging or personal phone calls from medical assistants with additional reminders.
In an effort to reduce disparities in screening rates between white patients and Latino patients, we provide all outreach, educational, and instructional materials in both English and Spanish.
‘Inreach’ Supports Outreach
To amplify our outreach campaign, we also employ communications strategies aimed at patients who are on-site in the medical office building. These “inreach” methods vary across our regions, but there is a common denominator: regardless of the reason for a patient’s visit, the EHR system can alert any staff member—whether a receptionist, medical assistant, or doctor—that the patient is due for a CRC screening when he checks in for an appointment. The staff member is empowered to remind the patient about the FIT kit that was mailed, and even to hand the patient a kit right then and there. In some offices, staff receive awards and prizes if they successfully help a patient complete a screening.
Patients can view a FIT kit how-to video in offices and online. In Northern California, we have also used our annual flu vaccination clinics as opportunities to remind targeted patients about CRC screening and to distribute FIT kits.
Outcomes: Leading the Nation
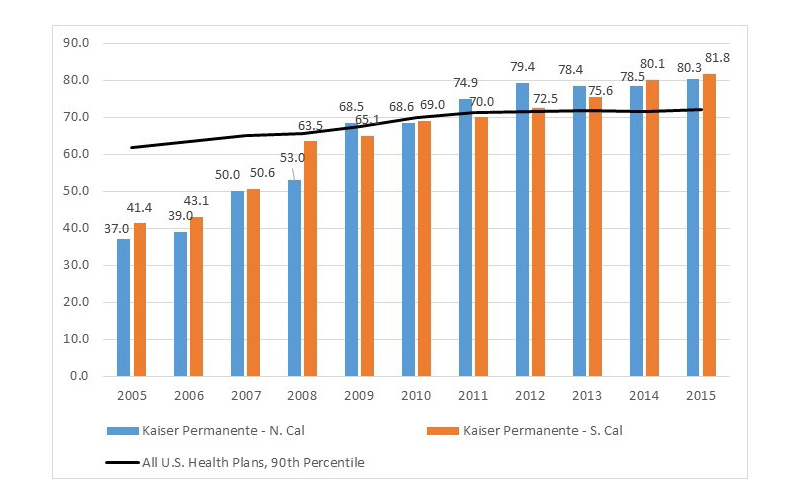
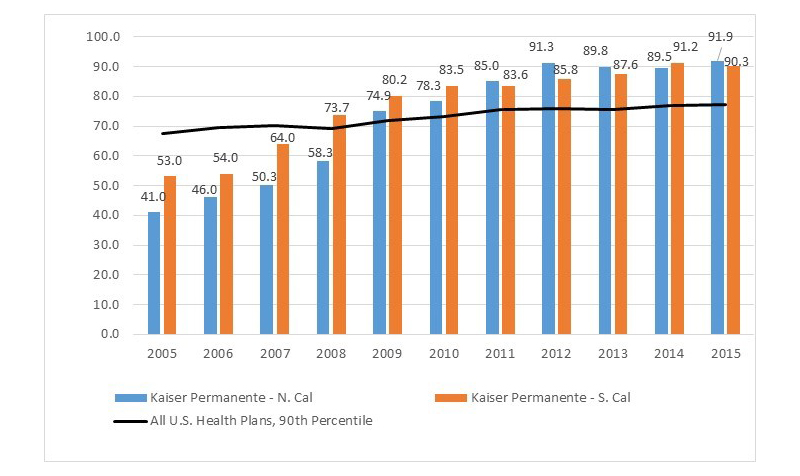
Kaiser Permanente’s efforts to improve CRC screening rates have paid off. Between 2005 and 2015, our commercial screening rates rose from 37 percent to just over 80 percent in Northern California, and from about 41 percent to almost 82 percent in Southern California (Figure 2). During the same time period, screening rates for our Medicare population rose from 41 to nearly 92 percent in Northern California, and from 53 to 90 percent in Southern California (Figure 3).
For both commercial and Medicare patients, we rank above the 90th percentile for screening rates among all U.S. health plans. This is true not only in California but in all of our regions. In 2014, the National Committee for Quality Assurance named our Mid-Atlantic region the best health plan in the nation for CRC screening rates for the Medicare population, and in 2015, our Northern California region held the number two spot in the nation.
With improved screening for any cancer, incidence rates initially rise as detection improves. However, because CRC screening also detects pre-cancerous polyps, which can be removed before becoming cancerous, a strong CRC screening program should eventually lead to a downward trend in cancer incidence in the screened population. This pattern has been evident at Kaiser Permanente. In Northern California we had 43 colorectal cancer cases per 100,000 patients in 2004 (before the intensive FIT kit outreach campaign), increasing to 53 per 100,000 when the program was fully implemented in 2008, and then declining to a low of 36 per 100,000 in 2015 (Figure 4).
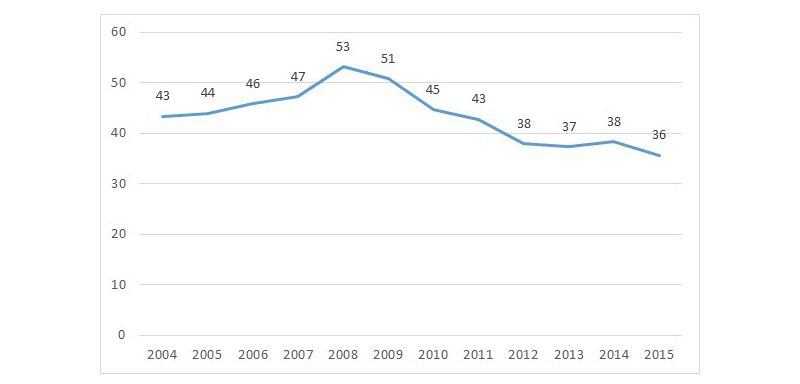
In addition to the lower incidence of colorectal cancer among the target population, preliminary analysis suggests that we are now finding cancers at earlier stages, when they are most treatable. Earlier-stage diagnosis results in less morbidity due to chemotherapy, better treatment outcomes, and more lives saved.
Conclusion
Screening rates are a product of two factors: offer rates and uptake/completion rates. With our FIT campaign we have made strides in both areas. With tools built into our EHR, we can now identify and offer tests to nearly 100 percent of the eligible population, practically with the touch of a button. At the same time, patient uptake of testing has improved dramatically, despite the fact that FIT screening must be done every year, instead of the five- and ten-year intervals required for sigmoidoscopy and colonoscopy, respectively. We believe the increased uptake is a testament to what happens when we “make the right thing easy to do,” for both doctors and patients. The test is easy; we put it directly into patients’ homes via their mailboxes and we keep it top-of-mind with multiple communications. We don’t (yet) have the technology to make all screening or primary care services this “easy,” but our experience with CRC screening gives us something to aspire to as we think about more efficient and effective ways of caring for our population.
There is a cost associated with our CRC screening outreach and inreach, but our capitated payment model enables us to direct resources toward these activities. Many value-based payment arrangements provide similar flexibility for delivery systems to invest in this type of outreach and inreach. As more and more delivery systems participate in payment arrangements that make them responsible for enrolled or attributed populations, we hope our experience provides useful lessons about reaching people before they become patients.
Theodore Levin, MD, is chief of Gastroenterology for the Diablo Service Area, Kaiser Permanente, and The Permanente Medical Group clinical lead for colorectal cancer screening; Joanne Schottinger, MD, is a medical oncologist and assistant medical director for Quality and Clinical Analysis for Kaiser Permanente Southern California; and Murray Ross, PhD, is a Kaiser Permanente vice president and director of the Kaiser Permanente Institute for Health Policy in Oakland. This post was originally published on the Health Affairs Blog and is reprinted with permission.


